Osteonecrosis in young adults is surprisingly common, with studies showing that 60% of patients are below 40 years of age. This serious bone condition, also known as avascular necrosis (AVN), occurs when blood supply to the bones diminishes, most frequently affecting joints—especially the femoral head. Men are particularly vulnerable, with a roughly 4:1 ratio compared to women, and a striking 77% of cases showing male dominance.
In fact, the impact on young lives can be devastating. While many believe bone diseases only affect older populations, the data tells a different story. For children and young adults aged 1-25, incidence rates range from 1-17.6%, with those aged 10-25 facing even higher risks—up to 61.1%. Furthermore, early warning signs like persistent joint pain, stiffness, and difficulty walking often go unrecognized until significant damage has occurred.
Throughout this article, we’ll explore why young adults develop osteonecrosis, how to identify the warning signs you shouldn’t ignore, and what treatment options exist. Understanding this condition is crucial because early intervention can significantly improve outcomes—especially considering that approximately 90% of patients achieve good functional results after appropriate treatment.
What is Osteonecrosis and Why It Matters for Young Adults
Bone death sounds alarming – and it is. Osteonecrosis, derived from the Latin words “ossis” (bone) and “necrosis” (killing or causing to die), literally means “bone death”. Also known as avascular necrosis (AVN), aseptic necrosis, or ischemic bone necrosis, this condition occurs when blood supply to a bone is interrupted or reduced.
Definition and affected joints
At its core, osteonecrosis is a degenerative bone condition characterized by the death of cellular components of bone secondary to an interruption of the subchondral blood supply. This disruption can lead to tiny breaks in the bone and eventually cause bone collapse. The process typically takes months to years and most commonly affects the ends (epiphysis) of long bones.
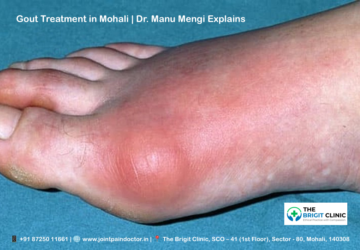
The hip (femoral head) stands as the most frequent site for osteonecrosis, followed by the knee and shoulder. Other affected areas include:
- The upper arm bone (humeral head)
- The ankle
- The wrist
- The foot
Moreover, osteonecrosis often affects the weight-bearing joints. In approximately 20% of cases, if one bone develops nontraumatic osteonecrosis, the same bone on the opposite side may also be affected, even without symptoms. For instance, if one hip has osteonecrosis, about 60% of the time the other hip is similarly affected.
Why young adults are increasingly at risk
Initially, many believe bone diseases primarily affect older populations. Nevertheless, osteonecrosis primarily strikes people between 30 and 50 years of age, making it a significant concern for young adults. Each year, an estimated 10,000 to 20,000 people develop osteonecrosis in the United States alone.
The risk factors specifically relevant to young adults include:
- Steroid use: High-dose corticosteroids (like prednisone) represent a common cause of osteonecrosis. For younger patients, this often relates to treatment for conditions like acute lymphoblastic leukemia, where studies show osteonecrosis developing in 2.5% of patients.
- Alcohol consumption: Chronic, excessive alcohol use (more than 13 ounces weekly for over 6 months) is a major risk factor. This can cause fatty deposits to form in blood vessels, reducing blood flow to bones.
- Trauma: Injuries such as dislocated joints or fractures can damage nearby blood vessels. Specifically, osteonecrosis occurs in 15% to 80% of patients with femoral neck fractures.
- Blood disorders: Conditions like sickle cell anemia and lupus can diminish vascular supply to bone. In patients with acute leukemia, studies indicate symptomatic osteonecrosis developing within a median of 1.8 years after diagnosis.
For this reason, osteonecrosis matters tremendously for young adults. The long-term implications are profound – joint collapse, premature osteoarthritis, persistent pain, and potential disability[20]. Additionally, since most hip replacements have a finite lifespan, young patients may face revision surgeries throughout their lifetime.
The unique susceptibility of adolescents and young adults isn’t easily explainable. One hypothesis suggests steroid therapy induces proliferation of marrow lipocytes. In adolescents with epiphyseal closure, this fat-cell hypertrophy results in elevated intraosseous pressure, reduced intramedullary blood flow, marrow ischemia, and ultimately, necrosis.
In view of these factors, early recognition and intervention become crucial for young adults. Without treatment, osteonecrosis typically leads to progressive deformity of affected joints, declining function, disability, pain, and premature osteoarthritis.
Common Causes of Osteonecrosis in Young Adults
Understanding what causes osteonecrosis can help young adults identify their risk factors early. Research indicates that in non-traumatic cases, alcohol abuse and corticosteroid use account for up to 80% of occurrences. Let’s examine the primary causes affecting young adults.
Steroid induced Osteonecrosis in young adults
Steroid use represents the most frequent non-traumatic cause of osteonecrosis. Between 9% and 40% of patients receiving corticosteroid treatment eventually develop this condition. The risk increases dramatically with long-term therapy, particularly with daily doses exceeding 15-20 mg.
The exact mechanism remains debated, albeit well-documented. Glucocorticoids directly affect bone cells by:
- Suppressing osteoblast precursor production
- Increasing apoptosis of osteoblasts and osteocytes
- Prolonging the lifespan of osteoclasts
Notably, certain patient populations face higher risks. Those with systemic lupus erythematosus, organ transplants, hematological diseases, multiple sclerosis, and SARS-CoV-2 infections show increased susceptibility. During the SARS epidemic of 2003, more than 1 in 5 patients developed osteonecrosis.
Even inhaled corticosteroids pose risks. Fluticasone propionate, commonly prescribed for chronic asthma, exhibits greater dose-related systemic effects than other inhaled steroids, particularly at doses exceeding 0.8 mg/day.
Alcohol related Osteonecrosis in young adults
Alcohol consumption represents another major risk factor, contributing to approximately 20-45% of osteonecrosis cases. The incidence in regular drinkers reaches as high as 5.3%.
Consequently, alcohol-induced osteonecrosis (AONFH) accounts for 32.4-45.3% of non-traumatic cases in Asia. The condition primarily affects men, with the male patient population roughly twice as large as the female population.
Alcohol damages bone through several mechanisms:
- Causing fat cell hypertrophy and proliferation
- Altering serum lipid levels
- Occluding blood vessels
- Increasing intraosseous pressure
These changes ultimately lead to inadequate blood supply and subsequent bone death. Furthermore, continued alcohol exposure worsens treatment outcomes, with 5-year survival rates after core decompression being lowest for alcohol-associated cases (22.1% versus 44.1% in idiopathic cases).
Traumatic Osteonecrosis in young adults
Trauma remains the most common overall cause of osteonecrosis. Femoral neck fractures or hip dislocations frequently disrupt blood flow to the femoral head. Accordingly, osteonecrosis occurs in 15-50% of femoral neck fractures and 10-25% of hip dislocations.
During these injuries, blood vessels supplying the femoral head become damaged, leading to interrupted circulation and eventual bone death. Unlike non-traumatic causes, the mechanism here is straightforward—direct physical damage to the vascular supply.
Non Traumatic Osteonecrosis in young adults
Beyond steroids and alcohol, several other non-traumatic factors can trigger osteonecrosis:
- Blood disorders: Sickle cell disease causes misshapen red blood cells that impede blood flow, making the femoral head particularly vulnerable.
- Autoimmune conditions: Systemic lupus erythematosus and other inflammatory disorders increase risk, sometimes regardless of steroid use.
- Coagulation abnormalities: Thrombophilia is a significant risk factor, with Factor V Leiden mutations present in approximately 10% of patients.
- Radiation therapy: About 20% of cases occur after radiation, though this has decreased to around 3% with optimized techniques.
Idiopathic Osteonecrosis in young adults
Despite extensive research, approximately 17-27% of osteonecrosis cases have no identifiable cause. These idiopathic cases present a challenge for both prevention and treatment.
Some researchers suggest genetic factors and gene polymorphisms may play roles in these unexplained cases. Regardless of the unknown cause, idiopathic cases show better outcomes than alcohol-related ones, with 5-year survival rates after core decompression at 44.1% compared to 22.1% for alcohol-associated cases.
Early Warning Signs You Shouldn’t Ignore
Recognizing the early signs of osteonecrosis can mean the difference between successful treatment and permanent disability. Given that osteonecrosis often progresses silently before causing noticeable symptoms, understanding these warning signals becomes essential, especially for young adults who might dismiss early discomfort as temporary or exercise-related.
Persistent joint pain or discomfort
The earliest and most common symptom of osteonecrosis is pain—often described as dull, throbbing, or aching. Typically, this discomfort begins gradually but becomes more intense over time. The pattern of pain offers important clues:
- Location-specific pain: Most commonly felt in the groin, thigh, or buttock when the hip is affected
- Activity-dependent pain: Initially present only during weight-bearing activities
- Progressive nature: Pain that steadily worsens, eventually occurring even at rest or at night
What makes this warning sign particularly tricky is that many young adults attribute this pain to overexertion or minor injuries. However, a key differentiating factor is persistence—pain that continues beyond a few weeks warrants medical attention, primarily if it follows any risk factors mentioned in previous sections.
Joint stiffness in young adults
As blood supply diminishes and bone tissue begins to die, stiffness emerges as a telltale indicator. This stiffness differs from ordinary morning stiffness or post-exercise tightness in several ways:
- It tends to be more pronounced after periods of inactivity
- Unlike muscle stiffness, it doesn’t typically improve with gentle movement
- The affected joint feels “locked” or resistant to normal range of motion
For young adults, joint stiffness might be easy to overlook or attribute to athletic activities. Yet persistent stiffness that limits everyday movements—such as difficulty putting on socks or shoes when hip osteonecrosis is present—should never be ignored.
Difficulty in walking in Osteonecrosis in young adults
As the condition progresses, walking becomes increasingly challenging. Obviously, this symptom varies depending on which joint is affected, but hip osteonecrosis (the most common type) creates distinctive walking difficulties:
- Altered gait: A noticeable limp or uneven walking pattern
- Weight-bearing limitations: Discomfort when putting weight on the affected side
- Need for support: Gradually increasing reliance on canes, crutches, or other walking aids
First thing to remember is that these walking difficulties often develop subtly. A young adult might first notice slight discomfort when climbing stairs, then find themselves avoiding longer walks, and finally experience difficulty with basic mobility. This progression rarely happens overnight but instead unfolds over weeks or months.
Reduced range of motion
The final warning sign—and one that strongly indicates advancing disease—is decreased joint mobility. This restriction happens as the joint surface becomes damaged and irregular due to bone death and collapse.
Reduced range of motion manifests in different ways depending on the affected joint:
- Hip: Difficulty or inability to rotate the hip inward or outward
- Shoulder: Limited ability to raise the arm overhead or reach behind the back
- Knee: Restricted bending or straightening capabilities
Essentially, this limitation often begins subtly—perhaps just a slight reduction in flexibility—but gradually becomes more pronounced and restrictive. Most importantly, unlike temporary stiffness that improves with stretching, the range-of-motion limitations in osteonecrosis tend to worsen over time rather than improve.
The key takeaway regarding these warning signs is their progressive nature. While individual symptoms might seem minor at first, their persistence and gradual worsening represent crucial red flags. Young adults experiencing any combination of these symptoms, particularly after exposure to known risk factors, should seek prompt medical evaluation rather than waiting until symptoms become severe or debilitating.
How Osteonecrosis is Diagnosed in Young Adults
Early diagnosis of osteonecrosis is crucial for preventing permanent joint damage in young adults. Currently, various diagnostic tools help clinicians identify this condition at different stages, with each offering specific advantages depending on when a patient seeks medical attention.
Physical examination and symptom history
The diagnostic journey typically begins with a thorough physical examination and comprehensive medical history. Although osteonecrosis may be asymptomatic in its early stages, making initial diagnosis challenging, a careful assessment can reveal important clues. Physicians should consider osteonecrosis primarily in younger patients presenting with joint pain who have known risk factors.
During the physical examination, doctors will assess:
- Range of motion limitations in the affected joint
- Pain with movement or weight-bearing
- Changes in gait or mobility
- Signs of joint swelling or tenderness
A focused medical history should explore potential risk factors, including:
- Recent steroid exposure
- Alcohol consumption patterns
- Previous trauma to the area
- Autoimmune conditions
- Blood disorders like sickle cell disease
- Recent orthopedic procedures
Screening of other joints is equally important, as osteonecrosis can affect multiple sites simultaneously. The risk of developing osteonecrosis in the contralateral hip when one side is affected ranges from 31% to 55%. In addition to the femoral head, osteonecrosis commonly affects the humeral head, femoral condyles, proximal tibiae, wrists, ankles, and bones of hands and feet.
X-Ray detection of Osteonecrosis in young adults
Plain radiographs (X-rays) are often the initial imaging tool used when evaluating suspected osteonecrosis. Although X-rays provide a readily accessible and inexpensive starting point, they have significant limitations for early-stage detection.
In the early phases, X-rays may show only minor osteopenia compared to the contralateral bone. As the disease progresses, characteristic findings emerge:
- Patchy areas of lucency with serpentine rims of sclerosis
- Sclerotic changes in small bones compared to adjacent structures
- The “crescent sign” – a linear crescentic subchondral lucency indicating imminent articular collapse
While helpful for excluding other causes of bone pain, standard radiographs generally confirm diagnosis only in more advanced stages of osteonecrosis. Furthermore, they frequently appear normal early in the disease course, potentially delaying proper treatment.
MRI for early detection of Osteonecrosis in young adults
Magnetic Resonance Imaging (MRI) stands as the gold standard for diagnosing osteonecrosis, with nearly 100% sensitivity and specificity for early detection. In contrast to X-rays and other imaging modalities, MRI can detect bone ischemia and osteonecrosis at an early stage, even when the patient remains asymptomatic.
The classic MRI findings in osteonecrosis include:
- Well-circumscribed geographic areas with distinct signal patterns
- Margins of low signal on T1-weighted and high signal on T2-weighted images (viable tissue)
- Alternatively, low signal on both T1 and T2-weighted images (necrotic tissue)
Most distinctively, the “double-line sign” serves as a diagnostic hallmark – an outer low signal and inner high signal circumscribing the affected area on T2-weighted sequences. This sign represents the outside rim of sclerosis and the reactive interface or “zone of creeping substitution”.
Beyond these established criteria, research has identified even earlier MRI signs that precede typical findings – subtle signal changes appearing as thin indistinct winding lines of T1 hypointensity with corresponding T2 STIR hyperintensity. These changes help predict subsequent development of extensive osteonecrosis on follow-up examinations.
At some institutions, all patients with acute lymphoblastic leukemia and bone marrow transplant recipients undergo MRI screening for early detection of osteonecrosis, regardless of symptoms. This proactive approach highlights the value of early identification, as MRI can detect changes as early as one week after vascular injury.
The presence of bone marrow edema on MRI is particularly significant, as it predicts worsening pain and future disease progression. Although MRI remains the optimal test for early diagnosis, its widespread use faces constraints due to higher economic costs and various contraindications. For this reason, physicians must carefully consider which patients warrant this advanced imaging based on risk factors and clinical presentation.
Stages of Osteonecrosis and What They Mean
Understanding the stages of osteonecrosis helps predict outcomes and guide treatment decisions for young adults. Regardless of which joint is affected, the disease follows a predictable pattern of progression that can be classified into distinct stages using various systems.
Stage 0 to Stage 4 overview
Several classification systems exist for staging osteonecrosis, with the Ficat and Arlet classification being one of the most widely used. This system combines clinical symptoms, radiographic findings, and MRI results to categorize the severity of bone damage:
Stage 0: This preclinical, silent stage shows normal imaging on both radiographs and MRI but may present abnormalities in bone marrow pressure and histology studies. Though asymptomatic, this stage can be detected if osteonecrosis has already been diagnosed in the contralateral joint.
Stage I: At this point, radiographs typically appear normal or show minor osteopenia. However, MRI reveals bone marrow edema, and patients often experience pain—typically in the groin for hip osteonecrosis. Bone scans at this stage show increased uptake, confirming the beginning of the disease process.
Stage II: As the condition advances, radiographs begin to show mixed osteopenia, sclerosis, and/or subchondral cysts, without any subchondral lucency. MRI displays a characteristic geographic defect. Clinically, patients experience increasing pain and joint stiffness.
Stage III: This critical stage marks the beginning of structural failure. Radiographs and MRI reveal the pathognomonic “crescent sign” indicating subchondral collapse. Subsequently, the femoral head (or other affected joint surface) begins to flatten. Pain intensifies, now radiating to surrounding areas like the knee in hip osteonecrosis, and patients develop a noticeable limp.
Stage IV: The final stage shows advanced degenerative changes on imaging. The joint space narrows significantly, and secondary changes appear in adjacent joint surfaces. Throughout this stage, pain becomes constant and mobility severely limited.
Some classification systems add additional stages. The Steinberg system, for instance, expands Ficat’s four stages into six stages and incorporates quantification of involvement within each stage—mild (less than 15% of articular surface), moderate (15-30%), or severe (greater than 30%).
Progression from silent to severe stages
The timeline of progression through these stages varies significantly among patients. Contrary to osteoarthritis, which typically develops slowly over many years, osteonecrosis often advances relatively quickly—within 12-18 months or sometimes over just a few months.
Initially, the disease begins silently. Young adults with stage 0 osteonecrosis experience no symptoms whatsoever. Henceforth, the condition evolves with subtle changes detectable only on MRI before progressing to produce noticeable symptoms.
Hip pain typically emerges as the first indicator. This discomfort usually presents as a dull ache or throbbing pain in the groin or buttock area. As bone deterioration continues, standing and weight-bearing become increasingly difficult, and joint movement causes significant pain.
The progression from stage I to stage IV creates a predictable pattern of disability:
- Early stages (0-I): Minimal or no symptoms, normal radiographs
- Middle stages (II): Increasing pain, visible changes on radiographs
- Advanced stages (III-IV): Joint collapse, significant pain, and functional limitations
Core decompression surgery demonstrates the best results when performed during early stages, before bone collapse occurs. In these cases, the bone can potentially heal and regain its blood supply. Straightaway after successful procedures, patients typically return to walking unassisted within approximately 3 months.
If diagnosed after collapse (stage III or beyond), core decompression generally proves unsuccessful in preventing further deterioration. At this point, total joint replacement often becomes the most viable option for relieving pain and restoring function.
Treatment Options: From Conservative to Surgical
Treatment decision-making for osteonecrosis hinges on timing and disease stage. Managing this condition effectively requires a stage-appropriate approach that balances joint preservation with long-term outcomes.
Conservative treatment Osteonecrosis in young adults
Non-surgical approaches serve as first-line interventions for early-stage osteonecrosis. These typically include:
- Restricted weight-bearing using canes, crutches, or walkers to delay disease progression, though evidence suggests reducing joint forces alone may not significantly slow advancement
- Pharmacological interventions such as bisphosphonates, statins, vasodilators, and anticoagulants target biological pathways involved in osteonecrosis
- Extracorporeal shockwave therapy (ESWT) stimulates osteoblastic activity, increasing bone density with most significant benefits seen in early disease stages
- Hyperbaric oxygen therapy (HBOT) enhances tissue oxygen partial pressures, stimulating osteoblasts and reducing inflammation, with protocols typically involving 60-90 daily sessions
Certainly, conservative approaches work best before femoral head collapse occurs. As a stand-alone strategy, non-surgical management generally serves as an interim solution rather than definitive treatment for most young patients.
Core decompression surgery in young adults
Core decompression remains the most widely performed joint-preserving procedure, creating channels within necrotic bone to relieve pressure and promote revascularization. This procedure shows optimal results when performed before femoral head collapse, with success rates varying from 34-95%.
The efficacy of core decompression correlates directly with disease stage. Patients with Ficat stage I disease demonstrate significantly better outcomes with approximately 80% success rates compared to those with stage III disease. Moreover, lesion size and location influence results—lateral or central lesions show higher failure rates than medial ones.
Recent technical improvements include multiple small-diameter drilling rather than single large core removal, reducing complications like subtrochanteric fractures. This modified approach has shown comparable efficacy with traditional methods while minimizing invasiveness.
Hip Replacement surgery in young adults
Once femoral head collapse occurs, total hip arthroplasty (THA) often becomes necessary. Presently, advances in implants and revision techniques have made THA viable even as initial treatment for young osteonecrosis patients.
Long-term studies show promising results—implant survival rates of 100% at 60 months, 98% at 120 months, and 94% at 180 months. Remarkably, when considering aseptic loosening as the endpoint, the 180-month survival rate reaches 100%.
Despite concerns about revision surgeries in young patients, modern implants demonstrate excellent durability. Correspondingly, clinical outcomes show high functionality, with median Japanese Orthopedic Association scores of 100 points at final follow-up.
Stem cell therapy for Osteonecrosis in young adults
Stem cell therapy, particularly using mesenchymal stem cells (MSCs), represents a breakthrough in biological treatment aimed at restoring bone structure and vascularity. This approach has emerged as a promising joint-preservation strategy for young adults.
Studies show that autologous cell therapy combined with core decompression significantly reduces femoral head collapse risk (odds ratio = 0.2) compared to decompression alone. Investigations demonstrate that stem cell therapy delivers superior clinical and radiological outcomes, especially in precollapse stages.
In long-term follow-up studies spanning up to 15 years, patients treated with bone marrow concentrate showed better survival time before revision than those receiving primary total hip arthroplasty. Furthermore, complications from stem cell procedures appear infrequent and primarily related to bone marrow aspiration.
Rehabilitation and Recovery After Treatment
After receiving treatment for osteonecrosis, young adults face another crucial phase – rehabilitation. The recovery process plays a vital role in determining long-term outcomes and quality of life. Let’s explore the key components of successful rehabilitation.
Physical therapy and mobility training
Physical therapy forms the cornerstone of rehabilitation for young osteonecrosis patients. Healthcare professionals typically recommend several approaches:
- Rest and weight restriction: Limiting weight-bearing activities or using crutches for several months helps slow bone damage progression. This reduced load gives the bone a chance to heal.
- Range-of-motion exercises: A physical therapist can teach specific movements to maintain or improve joint mobility. These exercises typically begin with passive movements and stretching before advancing to more active techniques.
- Progressive strengthening: As joint contractures improve, therapy shifts toward muscle-strengthening and endurance training. This step-by-step approach prevents overwhelming the healing joint while rebuilding necessary support.
- Gait training: Proper walking mechanics become crucial once weight-bearing is allowed. If limping persists, continued use of walking aids like canes may be recommended.
For hip osteonecrosis specifically, therapy focuses on the surrounding muscles – not just the joint itself. Strengthening exercises target hip, thigh, back, and core muscles that provide essential joint support.
Pain management strategies
Managing pain effectively enables better participation in rehabilitation activities. Several approaches work together:
Firstly, modalities like thermotherapy (heat) often provide significant relief for deep joint pain. Meanwhile, electrical stimulation represents another valuable option, working through two mechanisms: encouraging new bone growth and directly reducing pain.
In many cases, analgesic medications help control discomfort during early rehabilitation phases. Nevertheless, successful comprehensive rehabilitation can eventually eliminate the need for pain medication. Indeed, one case study documented complete discontinuation of tramadol after just 20 days of rehabilitation treatment.
Can young adults recover from Osteonecrosis in young adults?
Recovery prospects for young adults with osteonecrosis depend largely on early intervention, treatment approach, and rehabilitation compliance. Thus, physical therapy can be quite effective if osteonecrosis is detected early – though treatment aims to prevent further damage rather than reverse existing damage.
The recovery timeline varies based on treatment type. Following core decompression, patients typically return to unassisted walking within approximately 3 months. Afterward, progressive rehabilitation continues with gradually increasing intensity.
Success stories demonstrate remarkable potential for recovery. For instance, one documented case showed a young patient who, after comprehensive rehabilitation, experienced pain reduction from severe to minimal levels (NRS score of 1) without medications. Two years post-treatment, this individual had returned to work, married, had a child, and was leading an active social life.
The key to successful recovery lies in a multidisciplinary approach focused not just on eliminating pain but on empowering patients to better manage their condition through environmental adjustments and enhanced self-efficacy.
Prevention and Lifestyle Changes That Help
Preventing osteonecrosis starts with identifying modifiable risk factors that contribute to bone damage. Taking action early can protect young adults from this debilitating condition.
Quitting alcohol to prevent Osteonecrosis in young adults
As a matter of fact, alcohol abuse accounts for approximately 20-45% of osteonecrosis cases. The incidence in regular drinkers reaches as high as 5.3%. Even worse, continued alcohol exposure leads to inferior treatment outcomes, with 5-year survival rates after core decompression being merely 22.1% versus 44.1% in idiopathic cases. To minimize risk, experts recommend limiting alcohol consumption to one drink daily for women and two drinks daily for men.
Avoiding steroids in bone damage
In the long run, steroid use increases osteonecrosis risk by up to 20 times. Between 9% and 40% of patients receiving corticosteroid treatment eventually develop this condition. Under those circumstances, the most compelling evidence suggests tapering corticosteroids to the lowest necessary dose. If prescribed steroids, work closely with your healthcare provider to avoid long-term use whenever possible.
Monitoring bone health proactively
To be sure, maintaining strong bones requires a comprehensive approach. Consume a diet rich in calcium from dairy, nuts, and green vegetables. Vitamin D, either from sun exposure or supplements, remains equally crucial. Weight-bearing exercises like walking, dancing, or hiking help strengthen bones. Regular bone density testing may be recommended if you’re over 50 or have risk factors for bone loss.
Conclusion
Osteonecrosis represents a serious threat to young adults, though many still mistakenly view it as an older person’s condition. Throughout this article, we’ve seen how this bone death process disproportionately affects those under 40, particularly men. Early recognition of warning signs such as persistent joint pain, stiffness, and mobility limitations can significantly alter the disease trajectory.
Undoubtedly, the best outcomes occur when diagnosis happens before bone collapse. MRI technology now allows detection at the earliest stages, sometimes even before symptoms appear. This early identification means young patients can benefit from less invasive interventions like core decompression or emerging stem cell therapies rather than facing joint replacement surgery.
The stark reality remains that certain lifestyle factors dramatically increase risk. Alcohol consumption and steroid use stand as the two most significant modifiable risk factors, together accounting for up to 80% of non-traumatic cases. Young adults must therefore consider these connections when making health decisions.
Prevention strategies should focus on bone health maintenance through proper nutrition and weight-bearing exercise. Those already diagnosed must commit to comprehensive rehabilitation programs that strengthen surrounding muscles and restore proper movement patterns. Physical therapy, while challenging, offers the best path toward functional recovery.
Life after osteonecrosis diagnosis does not mean permanent disability for young adults. Modern treatment approaches combined with dedicated rehabilitation now provide much better outcomes than ever before. The key lies in awareness, early action, and appropriate treatment selection based on disease stage. Young adults experiencing unexplained joint pain should never dismiss their symptoms but instead seek prompt medical evaluation – because when it comes to osteonecrosis, time truly matters.
Key Takeaways
Osteonecrosis isn’t just an older person’s disease—it primarily affects young adults under 40, with early detection and intervention being crucial for preventing permanent joint damage and disability.
• Recognize the warning signs early: Persistent joint pain, stiffness, walking difficulties, and reduced range of motion are red flags that shouldn’t be dismissed as exercise-related discomfort.
• Address modifiable risk factors immediately: Alcohol abuse and steroid use account for 80% of cases—limiting alcohol and avoiding long-term steroids significantly reduces your risk.
• Seek MRI diagnosis before X-rays show damage: MRI can detect osteonecrosis weeks before symptoms appear, while X-rays only show advanced stages when treatment options become limited.
• Treatment success depends on timing: Core decompression and stem cell therapy show 80% success rates in early stages, but joint replacement becomes necessary once bone collapse occurs.
• Recovery requires comprehensive rehabilitation: Physical therapy, pain management, and lifestyle modifications enable young adults to return to active lives and prevent further joint deterioration.
The bottom line: Don’t ignore persistent joint pain if you have risk factors. Early intervention can mean the difference between preserving your natural joint and needing replacement surgery in your twenties or thirties.
FAQs
Q1. What are the early warning signs of osteonecrosis in young adults? Early signs include persistent joint pain, especially in the hip or knee, that worsens with weight-bearing activities. Other symptoms are joint stiffness, difficulty walking, and reduced range of motion. These symptoms often develop gradually over weeks or months.
Q2. What are the main causes of osteonecrosis in young people? The most common causes in young adults are excessive alcohol consumption and long-term use of high-dose corticosteroids. Traumatic injuries, blood disorders like sickle cell disease, and certain autoimmune conditions can also lead to osteonecrosis. In some cases, the cause remains unknown (idiopathic).
Q3. How is osteonecrosis diagnosed in its early stages? MRI is the gold standard for early diagnosis of osteonecrosis, capable of detecting changes even before symptoms appear. X-rays are often normal in early stages. A thorough physical examination and medical history, focusing on risk factors, are also crucial in the diagnostic process.
Q4. What treatment options are available for young adults with osteonecrosis? Treatment depends on the disease stage. Early-stage options include conservative measures like restricted weight-bearing and medications. Core decompression surgery and stem cell therapy show promise in preserving the joint. In advanced stages with bone collapse, joint replacement may be necessary.
Q5. Can lifestyle changes help prevent osteonecrosis in young adults? Yes, certain lifestyle changes can significantly reduce the risk. Limiting alcohol consumption, avoiding long-term use of high-dose steroids when possible, maintaining a healthy diet rich in calcium and vitamin D, and engaging in regular weight-bearing exercises can all contribute to better bone health and lower osteonecrosis risk.