Diabetic Foot complications affect approximately half of all people with diabetes who experience some form of nerve damage. These problems represent a major health concern and a common cause of hospitalisation. Without fast treatment, a toe, foot, or even part of the leg may require amputation, making timely orthopedic intervention critical for limb preservation. Dr. Manu Mengi, recognised as the Best Orthopedic Surgeon for Diabetic Foot Care in Mohali, emphasises that early specialist care can dramatically reduce the risk of amputation.
As orthopedic specialists, we regularly see how diabetic neuropathy and poor blood flow create serious risks for developing foot ulcers and infections. Additionally, conditions like Charcot foot disease can create deformities where bone is exposed directly under the skin surface, significantly increasing the risk of amputation. When diabetic patients develop an ulcer with Charcot foot, their amputation risk jumps to 50%, compared to just 10% without an ulcer.
In this comprehensive guide, we’ll explore our role as orthopedic surgeons in diabetic foot management, including reconstruction techniques, off-loading strategies, and collaborative approaches that help preserve function and prevent devastating complications.
Understanding Diabetic Foot Complications
Diabetic foot complications primarily stem from the long-term effects of persistently high blood sugar on nerves and blood vessels. These conditions develop gradually, often without noticeable symptoms until significant damage has occurred. Understanding these mechanisms is essential for early intervention and prevention of serious outcomes.
What causes diabetic foot problems?
The foundation of diabetic foot problems lies in blood sugar levels that remain elevated over time. This hyperglycemia damages both small and large blood vessels throughout the body, but the effects are particularly pronounced in the feet. Furthermore, the production of advanced glycation end products (AGEs) plays a crucial role in tissue damage. These compounds form when glucose binds to proteins and DNA, altering their structure and function.
Poor blood supply to the feet creates a perfect storm for complications. Essentially, two major pathways lead to foot problems: nerve damage that reduces sensation and blood vessel damage that impairs healing. The interaction between these factors means even minor injuries can develop into serious complications.
Nearly 15% of people with diabetes will eventually develop a foot ulcer, and damage can occur without the person ever noticing due to diminished pain sensation. Moreover, studies show that having an A1C over 7% for at least three years substantially increases your risk of developing diabetic neuropathy.
The role of diabetic neuropathy and poor circulation
Diabetic neuropathy manifests in several ways that directly impact foot health. Sensory neuropathy reduces protective sensation, making it difficult to feel cuts, blisters, or pressure points. Therefore, injuries often go unnoticed until they’ve become severe. Motor neuropathy affects muscle function, leading to foot deformities and abnormal pressure distribution when walking.
Perhaps most overlooked, autonomic neuropathy impairs sweat production, resulting in dry, cracked skin that’s more susceptible to injury. This creates easy entry points for infection. Unlike normal feet that signal pain when injured, neuropathic feet might continue bearing weight on damaged areas, worsening injuries.
Poor circulation compounds these problems by reducing blood flow to injured areas. Specifically, diabetes damages small blood vessels, limiting the delivery of oxygen, nutrients, and infection-fighting cells to wounds. This vascular insufficiency means:
- Wounds heal more slowly
- Infections spread more easily
- Tissues receive inadequate nutrition
- Antibiotics have difficulty reaching infection sites
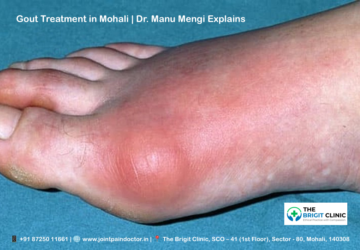
Common conditions: ulcers, infections, Charcot foot
Diabetic foot ulcers represent one of the most serious complications, affecting about 15% of diabetics during their lifetime. Unfortunately, these open wounds often develop silently on pressure points, especially under the foot. Once an ulcer forms, the race begins to heal it before infection sets in.
Infections in diabetic feet quickly become polymicrobial, involving multiple types of bacteria. Initially, they may start with common bacteria like Staphylococcus or Streptococci, but rapidly progress to include gram-negative and anaerobic organisms. Consequently, approximately 15% of ulcers develop osteomyelitis (bone infection), and of those, 15% require amputation.
Charcot foot, though affecting less than 1% of all people with diabetes, represents one of the most destructive complications. This condition develops when small injuries go unnoticed, allowing continued walking on damaged bones and joints. Over time, the foot’s architecture collapses, creating the characteristic “rocker-bottom” deformity.
The presence of Charcot deformity dramatically increases amputation risk. Specifically, diabetics with Charcot foot have a 50% chance of amputation if they develop an ulcer, versus only 10% without an ulcer. This stark difference highlights why early recognition and appropriate off-loading are critical in preventing catastrophic outcomes.
Early detection saves limbs! Visit the Best Hospital for Diabetic Foot Problems in Mohali for a thorough evaluation.
When Orthopedic Surgeons Step In
Proper timing of orthopedic intervention often makes the crucial difference between limb salvage and amputation for patients with diabetic foot complications. My experience shows that coordinated care yields dramatically better outcomes, with studies demonstrating that multidisciplinary approaches reduce ulcer recurrence rates from 58.4% to 30.4% over two years.
Referral criteria for orthopedic evaluation
Prompt orthopedic referral becomes necessary under several specific circumstances. Primarily, patients showing these red flags require immediate orthopedic evaluation:
- Active ulcerations, particularly those with signs of infection
- Traumatic injuries to the diabetic foot
- Suspected or confirmed Charcot foot
- Presence of a foreign body
- Signs of ischemia or gangrene
Additionally, patients with a history of previous ulceration or amputation fall into the highest risk category. Without preventive intervention, 58-83% of these patients will develop another ulcer within just one year. Nonetheless, with proper therapeutic footwear and insoles, this recurrence rate can be halved to 30-50% annually.
Besides acute presentations, orthopedic evaluation should be considered for patients showing no signs of wound healing within 4-6 weeks despite optimal management, regardless of initial vascular diagnostic test results.
Diabetic Foot in Orthopedics: scope and responsibilities
As orthopedic surgeons, our responsibilities in diabetic foot management encompass both preventive and reactive interventions. The foundation of our approach involves a thorough assessment of peripheral neuropathy, skin integrity, existing ulcers, foot deformities, vascular status, and footwear appropriateness.
Subsequently, our clinical work includes specialised surgical interventions like debridement, ray amputations, and corrective procedures for Charcot deformities. We also implement advanced wound healing technologies where appropriate. For instance, negative pressure wound therapy (NPWT) has emerged as one of the most effective current strategies for reducing amputation risk while increasing healing rates.
Orthopedic management further involves risk stratification and treatment planning based on the presence of peripheral neuropathy, foot deformity, and ulcer history. Correspondingly, we design individualised treatment plans combining patient education, orthoses, specialised footwear, and schedules for ongoing skin and nail care.
Multidisciplinary collaboration with endocrinologists and podiatrists
The complexity of diabetic foot disease necessitates collaborative care. A well-structured multidisciplinary team (MDT) typically includes specialists from medicine (endocrinology, infectious diseases, vascular surgery), podiatry, nursing, nutrition, orthotics, and physiotherapy.
In this collaborative model, podiatrists often serve as “gatekeepers” for prevention and management, with their specialised focus on biomechanics being particularly valuable. Their expertise in preventive strategies includes regular monitoring, routine care of calluses, and insole/shoe recommendations.
Meanwhile, endocrinologists manage the underlying metabolic condition, as glycemic control directly impacts wound healing. Studies demonstrate that comprehensive MDT approaches reduce hospital stays, decrease financial burden, and substantially lower amputation rates by 36-86%. Furthermore, patients managed by MDTs show faster wound healing times and lower severity of necessary amputations.
The International Working Group on the Diabetic Foot (IWGDF) recommends at least three levels of foot care management with interdisciplinary specialists. Under this framework, we coordinate with vascular surgeons for blood flow assessment, infectious disease specialists for antibiotic management, and endocrinologists for optimising glycemic control.
Overall, research consistently shows that MDT management yields superior outcomes to isolated speciality care. Accordingly, establishing clear communication channels between team members ensures seamless care coordination from hospital to community settings.
Need expert care for diabetic foot ulcers? Dr. Manu Mengi specialises in Diabetic Foot off-loading Techniques in Mohali and advanced limb-saving procedures.
Surgical Reconstruction Techniques in Diabetic Foot
Reconstructive surgery offers limb-saving options for patients with advanced diabetic foot conditions. With proper surgical intervention, we can often preserve function and mobility even in cases that might otherwise progress to major amputation.
Surgical Reconstruction in Charcot Foot
Charcot neuroarthropathy creates complex deformities that often require surgical reconstruction to preserve the foot. Although conservative management remains the first line of treatment, surgery becomes necessary when patients develop significant instability, ulceration, or deformity despite adequate offloading.
First and foremost, the timing of surgery is critical—ideally performed during the quiescent stage (Eichenholtz stage 2 or 3) of the disease process. Surgical techniques include internal fixation, external fixation, or a combination of both approaches. In essence, our goal is to achieve a stable, plantigrade foot resistant to ulceration.
Recent studies show that despite high complication rates, surgical reconstruction can achieve successful fusion in approximately 86% of cases. Nevertheless, complications directly attributable to the surgical technique occur in about 36% of patients. The post-reconstruction amputation rate remains relatively low at 5.5%, with 91% of patients returning to ambulation.
Arthrodesis of Diabetic Foot: when and why
Ankle arthrodesis (fusion) serves as a salvage procedure for diabetic patients with significant ankle instability or deformity. Indeed, tibiotalocalcaneal (TTC) fusion is commonly performed to address both ankle and hindfoot issues simultaneously.
Although considered an effective limb-salvage procedure, arthrodesis carries substantial risks. Studies report overall complication rates exceeding 75% in diabetic patients undergoing primary ankle arthrodesis. These complications include a 38.5% reoperation rate, 38.5% infection rate, and 23.1% amputation rate.
Rather than viewing these statistics as prohibitive, we use them to guide patient selection and counselling. Since patient selection significantly impacts outcomes, we carefully evaluate comorbidities and vascular status before recommending fusion procedures.
Ray Amputation in Diabetic Foot
Ray amputation involves removing a toe along with part of its corresponding metatarsal. This procedure provides an excellent option for ensuring adequate surgical debridement of infected margins while preserving foot function.
In contrast to major amputations, ray amputations show significantly lower mortality rates. Studies indicate the hazard rate is 1.6 times higher with major amputations compared to ray procedures. Furthermore, limb salvage can be achieved in almost two-thirds of patients undergoing minor amputations.
Appropriate patient selection remains crucial for success. Ideally, patients should have at least one palpable pedal pulse and adequate vascular indices. With proper selection, ray amputations show success rates of approximately 70%.
Managing Lisfranc Dislocation in Charcot Foot
Lisfranc joint involvement occurs in 45% of Charcot foot cases, making it the most common site affected in Charcot arthropathy. Although rare in the general population, Lisfranc injuries occur more frequently in diabetic patients and often follow minimal trauma.
Since these injuries can trigger or represent the first sign of an underlying Charcot process, careful evaluation is essential. MRI examination proves particularly valuable as radiographic findings are frequently subtle and easily missed. The oblique axial plane allows visualisation of the entire length of the Lisfranc ligament, providing crucial diagnostic information.
Arthrodesis vs Amputation Decision-Making in Diabetic Foot
When deciding between reconstruction and amputation, we consider several key factors:
- Vascular status – Adequate blood flow is essential for healing after reconstruction
- Extent of infection – Deep, uncontrollable infection may necessitate amputation
- Functional goals – Patient’s mobility needs and lifestyle considerations
- Overall health – Comorbidities that might affect healing potential
With this in mind, a strategic approach often involves performing the most distal amputation possible when necessary. This preserves length and function while removing infected or necrotic tissue. Although complications may occur, research shows that 80% of minor amputees remain alive after 2 years, with 64% maintaining full ambulation.
Worried about Charcot Foot Surgery in Mohali? Book a consultation with Dr. Manu Mengi to discuss minimally invasive options.
Off-Loading Strategies and Custom Orthotics
Off-loading remains the cornerstone of diabetic foot ulcer treatment, yet many clinics continue to use methods that haven’t been proven effective. Properly redistributing pressure away from vulnerable areas creates the foundation for successful healing and prevention of future complications.
What is off-loading, and why does it matter
Off-loading refers to relieving areas of elevated plantar pressure that contribute to diabetic foot ulcers. This pressure relief is crucial because studies show that uncomplicated plantar ulcers should heal within 6-8 weeks with adequate off-loading. Primarily, the goal is to redistribute weight evenly across the foot, reducing stress on bony prominences where ulcers commonly develop.
Even more importantly, effective off-loading prevents the “nutcracker effect” where continued pressure damages already vulnerable tissue. Unfortunately, patient adherence represents a major challenge—research shows patients use removable walking casts for only about 59% of their daily activity.
Custom Orthotics for Diabetic Foot
Custom orthotic devices play a vital role in managing diabetic foot by providing support, pressure relief, and protection. These specialised inserts are fabricated from breathable materials designed to cushion while supporting the ankle, arch, and heel.
Orthotic devices not only provide stability and limit joint movement but also help control foot deformities. For those with Charcot arthropathy, devices like the CROW (Charcot Restraint Orthotic Walker) orthosis completely cover the feet and legs, evenly distributing pressure to prevent ulcer development.
Total contact casting and removable boots
Total contact cast (TCC) remains the gold standard for off-loading diabetic foot ulcers. This specialised casting technique distributes weight along the entire sole by making close contact with its exact contours. A recent meta-analysis showed TCC provides higher healing rates (RR=1.22) and shorter healing time compared to removable devices.
As an alternative, removable knee-high walking boots offer similar benefits with greater convenience. The International Working Group on Diabetic Foot recommends a removable knee-high off-loading device with an adequate foot-device interface as first-choice treatment.
Preventing Joint Deformity in Diabetic Foot
Immobilisation alongside off-loading proves key to limiting structural damage. Certainly, early intervention with appropriate devices helps prevent the collapse of foot architecture commonly seen in Charcot arthropathy.
The patellar tendon weight-bearing (PTB) cast has shown promising results for stabilising joints affected by Charcot arthropathy with associated diabetic foot ulcers. This fibreglass cast reduces plantar pressure by facilitating load distribution across the entire plantar surface. Following initial treatment with PTB casting, patients typically transition to alternative removable off-loading devices over 3.5±1.9 months before gradually transferring to accommodative footwear over 6.1±1.8 months.
Looking for Custom Orthotics for Diabetic Foot in Mohali? Our clinic offers advanced solutions—schedule an appointment now!
Post-Surgical Care and Long-Term Management
Successful management of diabetic foot conditions extends far beyond the operating room. Consistent follow-up care, vigilant monitoring, and patient education form the foundation for long-term success after surgical intervention.
Diabetic Foot Debridement and Wound Care
Debridement plays a pivotal role in diabetic foot care as it removes nonviable tissue, facilitates wound healing, and helps prevent serious complications. This critical procedure can be performed through several methods, including sharp/surgical, enzymatic, autolytic, mechanical, and biological techniques.
Notably, removing devitalized tissues promotes angiogenesis and the development of granulation tissue, which accelerates healing timeframes. For optimal outcomes, we select the debridement method based on wound characteristics—surgical debridement for necrotic and infected wounds, enzymatic approaches for sloughy areas where surgery is contraindicated.
Research indicates that wounds decreasing their surface area by 20–40% within four weeks have a higher closure likelihood. Given that diabetes compromises immune function, timely debridement also limits the growth of pathologic organisms, including methicillin-resistant Staphylococcus aureus (MRSA).
Monitoring for Osteomyelitis in Diabetic Foot
Osteomyelitis (bone infection) requires vigilant monitoring as it significantly increases amputation risk. The treatment approach—surgical versus antibiotic therapy—remains individualised based on infection severity, vascular status, and patient factors.
Historically, complete surgical removal of infected bone was considered essential. Yet recent studies demonstrate that conservative treatment with prolonged antibiotic therapy can effectively promote wound healing and reduce major amputation risk. Conservative surgical approaches, where only infected bone is removed without amputation, show better outcomes in terms of ulcer healing (78% vs 57%) and healing time (181±30 days vs 462±98 days) compared to antibiotics alone.
Current guidelines suggest antibiotic therapy for 6 weeks if infected bone remains, but potentially just one week if properly resected. We generally consider osteomyelitis resolved when inflammatory markers decrease and radiological signs show positive evolution.
Education for Diabetic Foot Self-Care
Teaching patients proper self-care practices fundamentally reduces complication risks. Key recommendations include:
- Checking feet daily for cuts, redness, swelling, sores, or blisters
- Washing feet in warm (not hot) water and drying thoroughly
- Never going barefoot, even inside the home
- Wearing properly fitted shoes with socks
Temperature monitoring represents an innovative approach to early problem detection. Studies show that home temperature monitoring reduces ulcer incidence significantly—patients using infrared thermometers experience 8.5% ulcer occurrence versus 29.3% in standard therapy groups.
Preventing recurrence and future complications
Preventing recurrence requires diligent adherence to recommended practices. Primarily, therapeutic footwear and custom insoles serve as mainstays for preventing repeated ulceration. Even with optimal care, recurrence rates remain concerning—estimated at 40% within one year and 65% within three years.
Regular foot checks during healthcare visits plus annual podiatric evaluations form the cornerstone of prevention. Equally important, controlling blood glucose, blood pressure, and cholesterol helps minimise the risk of developing new complications.
Given that self-care may be the single most important factor in preventing complications, we ensure patients understand both the “how” and “why” behind recommended practices. This comprehensive approach—combining surgical intervention, careful monitoring, patient education, and preventive measures—offers patients the best chance for long-term foot health and mobility.
Prevent recurrence with expert care! Consult Dr. Manu Mengi, the Top Orthopedic Surgeon for Diabetic Neuropathy in Mohali, for lifelong foot health.
Conclusion
Diabetic foot complications represent a significant challenge in orthopedic practice, requiring specialised knowledge and a multidisciplinary approach. Throughout this article, we’ve examined how timely orthopedic intervention makes the critical difference between limb preservation and amputation. Therefore, understanding the complex interplay between neuropathy, vascular insufficiency, and mechanical stress remains essential for effective management.
The surgical techniques we’ve discussed—from ray amputations to complex arthrodesis procedures—offer viable options for patients facing serious complications. However, success depends on careful patient selection, meticulous surgical technique, and comprehensive post-operative care. Additionally, our approach must balance reconstruction against the sometimes necessary decision for amputation, always prioritising function and quality of life.
Off-loading strategies undoubtedly form the cornerstone of both prevention and treatment. Total contact casting continues to serve as the gold standard, though removable walking boots provide practical alternatives when applied correctly. Custom orthotics further enhance pressure redistribution, especially for patients with complex deformities or previous ulceration history.
Long-term management extends beyond surgical intervention, encompassing regular debridement, vigilant monitoring for osteomyelitis, and comprehensive patient education. Certainly, teaching patients proper self-care practices dramatically reduces recurrence rates and helps preserve mobility and independence.
As orthopedic surgeons, we play a crucial role within the multidisciplinary team addressing diabetic foot complications. This collaborative approach—combining our surgical expertise with specialised knowledge from endocrinologists, podiatrists, vascular surgeons, and wound care specialists—offers patients the best chance for successful outcomes. While diabetic foot complications present significant challenges, appropriate intervention combined with patient education and preventive measures can significantly reduce amputation rates and improve quality of life for patients living with diabetes.
Key Takeaways
Orthopedic surgeons play a critical role in diabetic foot management, offering specialised surgical interventions and off-loading strategies that can mean the difference between limb preservation and amputation.
• Early orthopedic referral is crucial – Patients with active ulcers, Charcot foot, or infection signs need immediate evaluation to prevent progression to amputation
• Multidisciplinary care reduces amputation rates by 36-86% – Collaboration between orthopedic surgeons, endocrinologists, and podiatrists delivers superior outcomes
• Total contact casting remains the gold standard for off-loading diabetic foot ulcers – providing higher healing rates than removable devices
• Surgical reconstruction can preserve limbs – Techniques like arthrodesis and ray amputation offer viable alternatives to major amputation in selected patients
• Patient education and self-care prevent 60% of recurrences – Daily foot checks, proper footwear, and temperature monitoring significantly reduce ulcer development
• Off-loading is the cornerstone of treatment – Proper pressure redistribution allows uncomplicated ulcers to heal within 6-8 weeks
The key to successful diabetic foot management lies in combining timely surgical intervention with comprehensive patient education and preventive strategies, ultimately preserving mobility and quality of life for patients with diabetes.
FAQs
Q1. What are the most effective off-loading techniques for diabetic foot ulcers?
A1. Total contact casting (TCC) is considered the gold standard for off-loading diabetic foot ulcers. It provides higher healing rates and shorter healing times compared to removable devices. Other effective techniques include removable knee-high walking boots and custom orthotics designed to redistribute pressure away from vulnerable areas.
Q2. How does surgical off-loading benefit patients with diabetic foot complications?
A2. Surgical off-loading can be beneficial for patients with Charcot neuroarthropathy deformities, especially when associated with infection and soft tissue loss. The goals of surgical off-loading include reducing hospital stays, minimising antibiotic therapy duration, decreasing surgical site complications, and achieving a stable, plantigrade foot.
Q3. What is the significance of the “50% rule” in diabetic foot wound management?
A3. The “50% rule” suggests that if a diabetic foot wound doesn’t decrease in size by at least 50% after four weeks of standard care (including infection control, optimised perfusion, pressure off-loading, and local wound care), it’s unlikely to heal within 12 weeks. This guideline helps clinicians determine when to consider alternative treatment strategies.
Q4. What role do orthopedic surgeons play in diabetic foot management?
A4. Orthopedic surgeons play a crucial role in diabetic foot management by providing specialised surgical interventions, implementing off-loading strategies, and participating in multidisciplinary care teams. Their expertise is particularly valuable in complex cases requiring reconstruction, managing Charcot foot deformities, and making decisions between limb salvage and amputation.
Q5. How can patients with diabetes best care for their feet to prevent complications?
A5. Patients with diabetes should check their feet daily for cuts, redness, swelling, or blisters. They should wash their feet in warm (not hot) water and dry thoroughly, never go barefoot (even at home), and wear properly fitted shoes with socks. Regular podiatric check-ups, blood glucose control, and using prescribed orthotics or therapeutic footwear are also essential for preventing complications.
About the Doctor
Dr. Manu Mengi is a highly skilled orthopaedic surgeon specialising in diabetic foot reconstruction and off-loading techniques in Mohali. With years of expertise in Charcot foot surgery, diabetic ulcer management, and limb salvage procedures, he is dedicated to providing cutting-edge treatments to prevent amputations and restore mobility.
Why Choose Dr. Manu Mengi?
✔ Best Orthopedic Surgeon for Diabetic Foot in Mohali
✔ Advanced diabetic foot reconstruction surgery at affordable costs
✔ Multidisciplinary approach for diabetic foot treatment in Mohali
✔ Personalised off-loading and orthotic solutions
Don’t let diabetic foot complications limit your life! Consult Dr. Manu Mengi, Mohali’s trusted diabetic foot specialist, today for expert care.