Post-COVID-19 Musculo-Skeletal Disorders affect millions of people worldwide since the pandemic began, causing significant health challenges beyond respiratory symptoms. The pandemic has negatively affected healthcare systems and caused both economic and social burden almost all over the world, with more than 6 million deaths recorded.
When we look at the data, musculoskeletal symptoms appear alarmingly frequent. In fact, studies show that fatigue affects up to 63% of COVID survivors, while muscle pain has a pooled prevalence of 28%. Additionally, joint pain affects 14.8% of patients even months after recovery. Many patients also report increased pain levels, with mean pain scores rising from 4.48 pre-COVID to 6.92 post-COVID. The most commonly affected areas include the lower back and shoulders. Although these symptoms might seem temporary, the prevalence of post/long COVID-19 syndrome ranges from 10% to 30%, indicating a significant long-term impact.
Throughout this article, we’ll explore how COVID-19 affects the musculoskeletal system, early symptoms to recognize, treatment options, and strategies for building an effective rehabilitation plan. Whether you’re currently experiencing these symptoms or helping someone who is, understanding these disorders is the first step toward effective management and recovery.
How COVID-19 Affects the Musculoskeletal System
Understanding the mechanisms by which COVID-19 disrupts our musculoskeletal system reveals a complex interplay of direct viral damage, inflammatory responses, and the consequences of reduced physical activity.
Direct viral effects on muscle and bone
The SARS-CoV-2 virus gains entry to human cells through angiotensin-converting enzyme 2 (ACE2) receptors and serum transmembrane protease 2 (TMPRSS2). Interestingly, these receptors are present not only in respiratory tissues but also in skeletal muscle and bone cells. This explains how the virus directly attacks musculoskeletal tissues.
Studies of muscle tissue collected from patients who died from SARS (a related coronavirus) revealed widespread muscle fiber atrophy with sporadic and focal muscle fiber necrosis. Under electron microscopy, researchers observed myofibril disarray and Z disk streaming, which significantly disrupts force transmission in muscles.
Beyond muscle damage, COVID-19 also affects bone health through direct viral action. Osteoclasts (cells that break down bone tissue) express ACE2 receptors, making them potential targets for the virus. Multiple animal studies have demonstrated dramatic bone loss following SARS-CoV-2 infection. For instance, mice infected with COVID-19 exhibited a 24.4% reduction in trabecular bone volume fraction in just two weeks, coupled with a 60% increase in osteoclast numbers. Notably, even asymptomatic mice displayed these significant changes, suggesting that immobility alone cannot explain the bone loss.
Immune response and inflammation
The inflammatory response to COVID-19 infection, particularly the “cytokine storm,” plays a crucial role in musculoskeletal damage. During this process, the body releases excessive amounts of proinflammatory cytokines that damage multiple organ systems, including muscles and bones.
Several inflammatory markers have been directly linked to musculoskeletal damage:
- C-reactive protein (CRP) levels in severe COVID-19 cases are often several-fold higher than in healthy individuals, correlating with muscle damage
- Interleukins (IL-1β, IL-6, IL-17) and tumor necrosis factor-alpha (TNF-α) directly induce muscle fiber breakdown while simultaneously decreasing protein synthesis
- These same inflammatory molecules can block the proliferation and differentiation of satellite cells—progenitor cells essential for muscle repair and growth
- IL-1β and IL-6 promote muscle fibrosis, impairing force production and increasing injury risk
Furthermore, the cytokine storm can lead to vascular damage in and around nerves and muscles. About 19% of hospitalized COVID-19 patients show elevated creatine kinase (CK) levels—a marker of muscle damage—with some cases reaching extremely high values (up to 12,216 U/L).
For bone health, inflammatory cytokines like CXCL10, IL-17, and TNF-α promote osteoclast activity while reducing osteoblast function (bone-forming cells), resulting in net bone loss.
Impact of prolonged inactivity
The COVID-19 pandemic forced many people into prolonged periods of inactivity due to lockdowns, hospitalization, or self-isolation. This lack of physical activity had profound negative effects on musculoskeletal health.
Physical inactivity is already highly prevalent in patients with rheumatic diseases (38-72%), but the pandemic exacerbated this problem for the general population. Even brief periods of reduced activity can be harmful—a two-week reduction in daily steps from approximately 10,000 to 1,500 steps leads to impaired insulin sensitivity, altered lipid metabolism, increased visceral fat, and decreased cardiovascular fitness in healthy adults.
For hospitalized COVID-19 patients, especially those requiring intensive care, the effects of immobility are even more severe. Bed rest, once considered beneficial for inflammatory conditions, is now known to accelerate joint destruction and muscle atrophy. Patients who recovered from SARS showed a 32% reduction in grip strength and a 13% decrease in six-minute walking distance 2-3 months after hospital discharge compared to healthy controls.
Moreover, during lockdown periods, people reported spending significantly more time watching television, using smartphones, and sleeping—all sedentary behaviors that correlate with increased musculoskeletal pain.
Recognizing the Symptoms Early
Identifying post-COVID musculoskeletal problems early allows for prompt intervention and better outcomes. As research continues to accumulate, distinct patterns of symptoms have emerged that can help both patients and healthcare providers recognize these conditions sooner rather than later.
Post-COVID fatigue and weakness
Physical fatigue stands out as the most prevalent long-term symptom following COVID-19 recovery, affecting more than 60% of individuals with long COVID. This isn’t ordinary tiredness—it’s often profound exhaustion that severely limits daily activities and can persist for months. Many patients describe a characteristic fluctuating pattern, where symptoms worsen unexpectedly after even minor physical exertion.
The underlying cause appears multifaceted. Research has revealed that COVID-19 can damage mitochondria (our cells’ power plants) and interfere with the electron transport chain that supplies energy to muscles. Subsequently, this leads to persistent weakness, reduced exercise tolerance, and rapid exhaustion. In more severe cases, patients demonstrate measurable declines in physical capacity—a study of recovered patients showed approximately a 32% reduction in grip strength and a 13% decrease in walking distance compared to healthy individuals.
Joint stiffness and pain
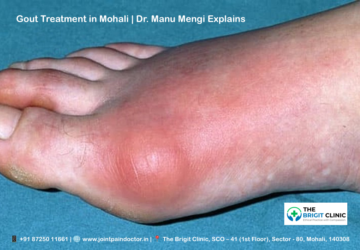
Joint pain (arthralgia) represents another hallmark of post-COVID musculoskeletal disorders, with prevalence rates ranging from 2% to 65% within the first year following infection. The knee, ankle, foot, and shoulders tend to be most frequently affected.
The pain experience varies considerably among individuals:
- 49.4% describe moderate intensity pain
- 26.1% report severe pain
- 4.9% experience very severe pain
This discomfort follows recognizable patterns—many patients notice their symptoms worsen in the morning and evening hours but improve somewhat with gentle exercise. Beyond mere discomfort, joint pain significantly impacts quality of life, with 88.9% of COVID survivors with persistent muscle/joint pain reporting reduced life quality compared to those without such symptoms.
Muscle cramps and tenderness
Muscle pain (myalgia) affects between 25% to 61% of long COVID patients, typically concentrated in the back, shoulders, and neck regions. Unlike some symptoms that appear immediately, muscle issues can emerge gradually, sometimes taking up to three months to fully manifest.
Interestingly, muscle biopsies from individuals experiencing persistent fatigue 5-14 months after infection reveal telling abnormalities—38% show muscle fiber atrophy while 56% display evidence of ongoing fiber regeneration. Electromyography tests frequently detect myopathic changes, with 75% of tested patients showing abnormal results consistent with muscle damage.
The nature of this pain resembles rheumatic conditions, leading some researchers to theorize that COVID-19 triggers an inflammatory response that mimics arthritis. Additionally, direct viral damage to motor neurons and adjacent muscles can occur during acute infection, potentially explaining why weakness persists long after the virus has cleared.
Sleep disturbance and fatigue
Sleep problems represent a frequently overlooked yet critical component of post-COVID recovery. Studies report vastly different prevalence rates ranging from 6% to over 70%, though one comprehensive international survey found 78.58% of long COVID patients suffered from sleep disturbances.
These problems manifest in various ways—difficulty falling asleep (39% vs. 31% pre-COVID), trouble staying asleep (57% vs. 43% pre-COVID), and increased reliance on sleep aids (30% vs. 24% pre-COVID). Moreover, patients report feeling less rested upon waking and an increased need for daytime napping.
Concerningly, these sleep disruptions prove stubbornly persistent, with 28% of patients still experiencing symptoms beyond 12 months after infection. Given sleep’s crucial role in musculoskeletal recovery, these disturbances create a troubling cycle—poor sleep impairs healing, which causes pain, which further disrupts sleep.
The combined effect of these symptoms can be devastating, with multiple studies showing significant negative impacts on quality of life, work capacity, and social functioning.
The Role of Inflammation and Immune Dysregulation
Immune system dysregulation represents a fundamental driver of post-COVID musculoskeletal disorders, with inflammation playing a central role in both acute and chronic phases of the illness. Beyond the initial infection, these immune abnormalities can persist for months, creating a cascade of effects throughout the body’s connective tissues.
Cytokine storm and tissue damage
The term “cytokine storm” describes the excessive activation of immune cells and significant increase in circulating cytokines that characterizes severe COVID-19 cases. This overwhelming inflammatory response creates a vicious cycle as abundant inflammatory cytokines cause profound hyper-inflammation and mobilize immune cells.
Within damaged muscle tissue, this storm elevates cytolytic and cytotoxic molecules along with reactive oxygen species (ROS), which aggravates tissue injury—sometimes extending to healthy nearby tissues. Severe inflammation in skeletal muscles can progress to rhabdomyolysis, potentially causing sepsis-like systemic inflammatory response syndrome and remote organ damage.
The mechanics of this damage are intricate. After initial injury, both local and recruited immune cells activate at the injured site. These activated lymphocytes, macrophages, and neutrophils contain radical-forming enzymes in their intracellular granules that generate ROS, which further increases tissue injuries and enhances immune responses. Concurrently, pro-inflammatory cytokines released from activated phagocytes accelerate muscle protein degradation.
Should tissue damage become prolonged and repair fails, a protein called HMGB1 released by necrotic tissues and immune cells induces a second wave of inflammatory responses, establishing chronic inflammation. This continuous inflammation contributes to various inflammatory diseases, which in turn stimulate more damage-associated molecular patterns (DAMPs), creating an ongoing destructive cycle.
Persistent low-grade inflammation
Many long COVID patients demonstrate a condition called low-grade inflammation (LGI)—a chronic, ineffective inflammatory state that leads to oxidative stress and causes ongoing tissue damage. In fact, approximately two-thirds of long COVID patients have persistently high levels of certain inflammatory signals.
This persistent inflammation differs significantly from those who recovered fully from COVID-19. In individuals who recovered completely, inflammation levels initially increased during infection but subsequently normalized as they healed. However, in those with long COVID, these inflammatory levels never returned to baseline.
LGI manifests through common symptoms including chronic fatigue, arthralgia, myalgia, anxiety, depression, and digestive issues. The underlying biological mechanisms involve slight elevations of acute-phase reactants and cytokines. A meta-analysis of 23 studies evaluating 18 inflammatory biomarkers revealed that C-reactive protein (CRP), lactate dehydrogenase (LDH), D-dimer, and leucocytes remained elevated in long COVID patients compared with those who recovered fully.
Interestingly, fatigue—the most prevalent symptom of post-COVID syndrome—correlates directly with high levels of erythrocyte sedimentation rate (ESR), LDH, CRP, and D-dimer. This association may be explained by the production of reactive oxygen species by activated neutrophils, which causes oxidative tissue damage.
Autoimmune responses and flare-ups
Perhaps most concerning is COVID-19’s apparent ability to trigger autoimmune responses. Approximately 9.5% of COVID-19 survivors report developing autoimmune diseases post-infection, with systemic lupus erythematosus being most frequent (75% of autoimmune cases), followed by rheumatoid arthritis (19%) and autoimmune thyroiditis (6%).
Research demonstrates an alarming 42.6% increased risk of autoimmune diseases among chronic COVID patients. More specifically, studies have identified a 3.2-fold increased risk of ankylosing spondylitis, a 3.14-fold greater risk of mixed connective tissue disease, a 2.99-fold higher risk of lupus erythematosus, and a 2.98-fold increased risk of rheumatoid arthritis.
The molecular basis for this autoimmunity involves SARS-CoV-2’s multiple epitopes that cross-react with host antigens. For example, researchers have shown cross-reactivity between SARS-CoV-2 epitopes and those on heat shock proteins, which could contribute to autoimmune conditions. Remarkably, up to 45% of COVID-19 patients exhibit at least one circulating autoantibody, with higher concentrations often resulting in more severe symptoms.
When Medications Make It Worse
Medications prescribed during COVID-19 treatment can sometimes worsen musculoskeletal problems, creating a challenging paradox for both patients and healthcare providers. While certain drugs proved life-saving during acute infection, their lasting impact on muscle and bone health requires careful consideration.
Steroid-related muscle and bone loss
Corticosteroids emerged as cornerstone treatments during the pandemic, yet their musculoskeletal side effects can be significant. These medications, despite saving countless lives, come with substantial risks to bone and muscle integrity. The main adverse effects include myopathy, muscle atrophy, muscle weakness, and osteonecrosis.
Prolonged steroid use frequently leads to glucocorticoid-induced osteoporosis, which dramatically increases fracture risk. Beyond this, avascular necrosis (AVN) of the femoral head represents one of the most devastating complications. Even with the low-dose dexamethasone protocol from the RECOVERY trial (equivalent to approximately 400 mg of prednisone), patients remain vulnerable. Remarkably, some patients developed osteonecrosis with cumulative prednisone doses as low as 290-400 mg.
Risk factors for steroid-induced complications appear dose-dependent:
- Each 10 mg increase in daily steroid dose correlates with approximately 3.6% higher rates of osteonecrosis
- Risk increases 1.57 times per 5.0 g increase in cumulative steroid dose
- Each additional 10 days of treatment duration increases osteonecrosis risk by 1.29 times
A proposed risk stratification system categorizes patients as low-risk (no steroids), moderate-risk (cumulative dose <2000 mg for <1 week), or high-risk (≥2000 mg for ≥1 week or IV pulse ≥80 mg/day for ≥3 days).
NSAIDs in musculoskeletal pain: pros and cons
Non-steroidal anti-inflammatory drugs remain widely used for managing COVID-19 symptoms like fever, body aches, and headaches. Early pandemic concerns about their safety have largely been resolved through extensive research.
According to current evidence, NSAIDs provide several benefits in COVID-19 management:
- Affordable and readily available over-the-counter
- Well-established benefit-risk profile
- Essential for managing chronic inflammatory conditions
The overwhelming majority of 24 relevant publications showed that NSAIDs neither increase SARS-CoV-2 infection likelihood nor worsen clinical outcomes. Furthermore, a meta-analysis demonstrated no increased mortality risk among NSAID users versus non-users.
Nevertheless, certain precautions remain advisable. The European Union’s National Treatment Guidelines recommend patients with COVID-19 can continue NSAIDs, yet advise using the lowest effective dose for the shortest required time. This balanced approach recognizes both benefits and potential concerns without contradicting their overall safety profile.
Other drugs linked to muscle weakness
Several other medications commonly prescribed during COVID-19 have been associated with musculoskeletal complications. Hydroxychloroquine/chloroquine, initially used widely before later studies showed limited efficacy, can cause myopathy as a primary adverse effect. Similarly, azithromycin, often chosen for pulmonary infections, carries potential muscle weakness risks.
Concerning statins, research indicates COVID-19 infection may intensify typical statin-related side effects. A study of 66 COVID-19 patients found those using statins experienced more frequent and intense muscle pain compared to controls. Additionally, muscle weakness occurred more frequently in statin users, and creatine kinase levels were higher, often correlating with moderate to severe muscle pain.
Certain antiviral treatments also present musculoskeletal risks. Studies report that lopinavir/ritonavir can lead to musculoskeletal pain and fatigue, while both interferon α and β have been linked to arthralgia and myalgia in some patients.
Given these potential complications, medication management requires careful consideration of individual risk factors, especially in patients already experiencing post-COVID musculoskeletal symptoms.
Living with Long COVID Muscle Pain
Living with long COVID muscle pain transforms everyday activities into significant challenges. The persistent symptoms extend far beyond occasional discomfort, creating a new reality for those affected by Post-COVID-19 Musculo-Skeletal Disorders.
How it affects daily life and mobility
The impact of long COVID on daily functioning is profound. Approximately 72% of COVID-19 survivors report long-lasting clinical complications. Among the most debilitating are fatigue (47.9%), muscle and joint pain (35.5%), and shortness of breath (34.7%). Consequently, these symptoms severely restrict normal activities.
Studies reveal that 75.5% of affected individuals report problems performing daily activities. Even basic self-care becomes challenging, with 64% of patients experiencing functional impairment. Physical health scores drop significantly in those with persistent pain, creating a vicious cycle of decreased activity and worsening symptoms.
Many describe their condition as having “strange,” “energy-sapping,” and often fluctuating muscle weakness that dramatically limits mobility. At the most extreme, some patients become essentially bedridden, unable to participate in previously routine activities. This has substantial economic implications as many affected individuals cannot maintain their previous work capacity.
Exercise intolerance after COVID
Exercise intolerance—the inability to perform physical activity at previously normal levels—emerges as a hallmark feature of long COVID. This manifests as dramatically reduced exercise capacity, with patients showing significant decreases in the six-minute walking test (6MWT) distances compared to those without long COVID.
In one study, individuals with long COVID walked an average of only 448 meters in the 6MWT, whereas fully recovered individuals averaged 509 meters. This difference reflects serious physiological impairments rather than just deconditioning.
The mechanisms behind exercise intolerance are multifaceted:
- Damaged mitochondria disrupting energy production in muscle cells
- Impaired diffusion capacity limiting oxygen utilization
- Persistent microthrombi in muscle capillaries reducing blood flow
- Altered muscle fiber composition favoring easily fatigable fibers
Exercise often triggers what’s called post-exertional malaise—a worsening of symptoms after even modest exertion. This leads to “boom-bust” cycles where patients push themselves on good days, essentially resulting in relapses that further limit future activity.
Postural orthostatic tachycardia syndrome (POTS)
POTS represents a frequently overlooked yet common autonomic dysfunction in long COVID patients. It affects approximately 31% of individuals with long COVID. This condition manifests as an abnormal heart rate increase upon standing—specifically a rise of ≥30 beats per minute within 10 minutes of standing, often exceeding 120 beats per minute, without corresponding blood pressure drops.
POTS disproportionately affects younger individuals, primarily women. In one study, POTS patients were significantly younger (average age 40.0 years) than non-POTS long COVID patients (47.0 years), with 91% being female.
During walking tests, POTS patients show significantly higher heart rates both during exercise and recovery periods. Their physical activity levels are markedly lower than other long COVID patients, as measured by standardized scales.
The condition creates a troubling cycle: orthostatic intolerance leads to decreased activity, which causes cardiovascular deconditioning, which then worsens POTS symptoms. Many patients with POTS report being unable to stand for prolonged periods, experiencing dizziness, fatigue, and palpitations that severely limit normal activities.
For most individuals, these musculoskeletal challenges of long COVID represent an ongoing struggle requiring comprehensive management approaches and lifestyle adaptations.
Understanding the Psychological Side of Pain
Beyond physical symptoms, the psychological impact of post-COVID musculoskeletal disorders creates an additional burden for patients. The mind-body connection plays a crucial role in how pain is perceived, processed, and managed.
Depression and anxiety in chronic pain
The mental health toll of Long COVID extends far beyond temporary emotional distress. Research shows that between 6% and 18% of COVID-19 survivors develop post-traumatic stress disorder (PTSD) within three months of recovery. More broadly, anxiety and depression rank as the most prevalent psychiatric outcomes 6-12 months post-infection.
Indeed, the psychological burden for COVID survivors is multifaceted—encompassing direct disease impacts, long-term health consequences, and social implications. This creates what researchers call a “vicious cycle” where pain exacerbates mental health issues, which in turn intensify pain perception.
Studies demonstrate that COVID-19 survivors experiencing social difficulties have heightened risk for anxiety and depression. For instance, Black individuals with Long COVID showed increased anxiety and depression related to financial burdens, employment challenges, food insecurity, and housing instability. This underscores how socioeconomic vulnerabilities compound psychological distress.
The relationship between back pain and mental health deterioration during the pandemic illustrates this connection. People with chronic back pain were 3.5 times more likely to develop anxiety and 1.8 times more likely to develop depression compared to those without such pain.
Fear of movement and kinesiophobia
One particularly troubling psychological phenomenon among COVID survivors is kinesiophobia—the irrational fear of movement. Patients with post-COVID syndrome score significantly worse on the Tampa Scale for Kinesiophobia compared to control groups.
This fear creates a paradoxical situation: patients avoid movement to prevent pain, yet this avoidance ultimately worsens their condition. As movement decreases, muscle weakness increases, creating a downward spiral of physical deterioration.
The origins of this fear may be rooted in traumatic illness experiences. Some patients report “freezing” with trembling limbs during activities—physical manifestations of psychological distress. Others describe how fear prevents them from attempting normal activities, leading to further deconditioning.
Interestingly, functional movement disorders sometimes develop as expressions of the inability to communicate fear verbally, forcing patients to express it through their bodies instead. This explains why some patients develop tremors and abnormal movements during isolation periods even after recovering from the virus itself.
Cognitive fatigue and brain fog
Among the most distressing psychological symptoms is “brain fog”—a colloquial term describing significant neurocognitive impairment affecting thinking, information processing, and concentration. Approximately 7.2% of COVID survivors report this debilitating symptom.
Cognitive difficulties manifest in various ways:
- Inability to multitask
- Difficulty processing information
- Forgetfulness
- Problems with focus and concentration
Alongside mental fatigue, reduced activity in specific brain regions (particularly the left superior temporal gyrus) correlates with cognitive deficits. Some evidence suggests the SARS-CoV-2 virus disrupts brain homeostasis through neuroinflammatory mechanisms that persist beyond viral clearance.
A particularly concerning discovery is blood-brain barrier disruption, which can persist up to a year after infection. Research using specialized MRI techniques found evidence of a “leaky” blood-brain barrier in participants with Long COVID brain fog, often associated with reduced global brain volume.
For most patients, brain fog eventually resolves within 6-9 months, though for some it persists 18 months or longer. Risk factors for developing brain fog include female sex, respiratory problems during initial infection, and ICU admission.
The combination of physical pain, psychological distress, and cognitive dysfunction creates significant challenges for COVID survivors. Effective treatment must correspondingly address both the physical and psychological dimensions of recovery.
What Helps: Treatment and Recovery Options
Effective recovery from post-COVID musculoskeletal disorders typically requires a multi-faceted approach tailored to individual symptoms and severity. Fortunately, research has identified several evidence-based strategies that can significantly improve outcomes for those struggling with persistent symptoms.
Physiotherapy and graded exercise
Physiotherapy stands as a cornerstone treatment for addressing long COVID musculoskeletal issues. Studies demonstrate that tailored exercise programs can improve not only muscle strength but also flexibility and cardiovascular fitness. Therapists often employ manual therapy to enhance joint mobility and reduce pain in patients experiencing musculoskeletal discomfort.
Interestingly, inspiratory muscle training has shown particularly promising results. In studies lasting at least 6 weeks, participants demonstrated statistically significant improvements in physical function. For instance, a 12-week home program of inspiratory muscle training yielded substantial benefits for respiratory function.
Importantly, exercise must be carefully calibrated. Experts recommend starting at low to moderate intensity with limited duration, typically scoring no higher than 4/10 on the Borg Scale CR10 for shortness of breath and fatigue.
Anti-inflammatory treatment in long COVID
Among available anti-inflammatory approaches, metformin shows the strongest clinical evidence with substantial reductions in long COVID incidence (42% to 63%). Additionally, low-dose naltrexone (LDN) demonstrates effectiveness in improving fatigue, post-exertional malaise, and pain.
Other promising options include:
- Dexamethasone, which reduces fatigue by 33% and shortens median symptom duration (133 days vs. 271 days)
- Omega-3 fatty acids for improving mental health and musculoskeletal symptoms
- L-Arginine combined with vitamin C, with 94.9% of patients reporting absence of fatigue
Nutritional support and hydration
Research indicates a 40% prevalence of at least one micronutrient deficiency among patients with post-COVID musculoskeletal manifestations. Iron, copper, and selenium deficiencies significantly correlate with symptom severity.
The arthritis group specifically showed higher prevalence of deficiencies compared to those with mild symptoms: iron (52.3% vs. 35%), selenium (56.5% vs. 14.1%), and copper (56.5% vs. 3.3%). Zinc plays a crucial role in immune modulation, with deficiencies leading to reduced natural killer cells and impaired immunity.
Pain education and pacing strategies
Educating patients about energy conservation and pacing represents a fundamental component of recovery. Physical therapists provide essential guidance on avoiding overexertion while optimizing daily activities. This approach helps manage the characteristic fluctuating nature of symptoms.
Proper pacing helps break the “boom-bust” cycle where patients overexert themselves on good days, leading to subsequent crashes. Accordingly, the goal is integrating physical activity into daily routines rather than treating it as a separate task, leading to more sustainable improvement.
Building a Personalized Rehab Plan
Creating a tailored rehabilitation program represents a crucial step for recovering from post-COVID musculoskeletal disorders. A systematic approach helps patients move from assessment to measurable recovery.
Assessing baseline function
A comprehensive evaluation forms the foundation of effective rehabilitation. Healthcare providers should conduct thorough history and physical examinations focusing specifically on functional status. Standardized assessment tools prove invaluable at this stage:
- WHO post-COVID-19 functional scale for overall function
- Montreal Cognitive Assessment (MOCA) for cognitive impairments
- Barthel Index for activities of daily living (higher scores indicate greater independence)
- Functional Independence Measure (FIM) for measuring recovery gains
Setting realistic goals
Rehabilitation goals must be highly individualized, addressing specific needs, resources, and abilities of each person. Firstly, healthcare providers should establish feasible short and long-term goals after thorough discussion with the patient and caregivers. As a matter of fact, shared decision-making empowers patients and increases adherence to rehabilitation plans.
Tracking progress and setbacks
Regular monitoring enables timely adjustments to rehabilitation strategies. Patients should be assessed at 12 weeks post-discharge with evaluations including chest X-ray, pulmonary function tests, and 6-minute walking tests. Henceforth, multidisciplinary teams can modify programs based on outcomes. Importantly, post-exertional symptom exacerbation and orthostatic hypotension require careful monitoring during exercise to prevent setbacks.
Conclusion
Post-COVID Musculo-Skeletal Disorders represent a significant health challenge affecting millions worldwide. Though originally perceived as primarily a respiratory illness, COVID-19 clearly impacts multiple body systems, particularly the musculoskeletal framework. The evidence points to a complex interaction between direct viral damage, inflammatory responses, and inactivity-related deconditioning that collectively contributes to persistent symptoms.
Many patients face a challenging journey from diagnosis through recovery. Fatigue, muscle weakness, joint pain, and sleep disturbances often persist long after the acute infection resolves. Additionally, these physical symptoms frequently coincide with psychological challenges such as depression, anxiety, and kinesiophobia, creating a multifaceted condition requiring comprehensive care.
Understanding the underlying mechanisms proves essential for effective management. The cytokine storm and persistent low-grade inflammation damage tissues and potentially trigger autoimmune responses, while medications used during treatment sometimes worsen musculoskeletal problems rather than alleviating them.
Recovery typically requires a tailored, multidisciplinary approach. Physiotherapy with carefully graded exercise, anti-inflammatory treatments, nutritional support, and pain education all play crucial roles in rehabilitation. Most importantly, patients must establish realistic goals based on thorough baseline assessments while tracking progress regularly.
The path toward recovery might seem daunting, yet proper management strategies offer real hope. Patients who follow structured rehabilitation programs generally show measurable improvements over time. Healthcare providers must recognize both the physical and psychological dimensions of these disorders while adapting treatment plans to individual needs.
Post-COVID musculoskeletal disorders will undoubtedly remain a significant health concern for years to come. Nevertheless, continued research and evolving treatment protocols promise better outcomes for those affected. Through early intervention, comprehensive care, and patient-centered approaches, those suffering from these debilitating conditions can find meaningful relief and gradually reclaim their quality of life.
Key Takeaways
Post-COVID musculoskeletal disorders affect millions globally, with symptoms persisting months after recovery. Understanding these complex conditions and implementing proper management strategies can significantly improve patient outcomes and quality of life.
• COVID-19 directly attacks muscles and bones through ACE2 receptors, causing fiber damage and bone loss even in asymptomatic cases • Persistent inflammation drives ongoing symptoms with cytokine storms creating chronic low-grade inflammation that damages tissues for months • Early recognition is crucial – fatigue (63%), muscle pain (28%), and joint pain (14.8%) are key warning signs requiring prompt intervention • Exercise intolerance and POTS are common affecting 31% of long COVID patients, creating cycles of deconditioning and worsening symptoms • Comprehensive treatment works best combining graded physiotherapy, anti-inflammatory medications, nutritional support, and pacing strategies • Personalized rehabilitation plans are essential with baseline assessments, realistic goals, and regular progress monitoring for optimal recovery
Recovery requires patience and multidisciplinary care, but structured rehabilitation programs show measurable improvements over time. The key is addressing both physical symptoms and psychological impacts through evidence-based approaches tailored to individual needs.
FAQs
Q1. What are the most common musculoskeletal symptoms experienced after COVID-19? The most common post-COVID musculoskeletal symptoms include fatigue (affecting up to 63% of survivors), muscle pain (28%), and joint pain (14.8%). Many patients also report weakness, stiffness, and reduced exercise tolerance.
Q2. How long can musculoskeletal symptoms persist after recovering from COVID-19? Musculoskeletal symptoms can persist for months after the initial COVID-19 infection. Some patients experience symptoms for 6-9 months, while others may have issues lasting 18 months or longer. The duration varies significantly between individuals.
Q3. Can COVID-19 trigger autoimmune responses in the body? Yes, COVID-19 can trigger autoimmune responses. Approximately 9.5% of COVID-19 survivors report developing autoimmune diseases post-infection, with conditions like systemic lupus erythematosus, rheumatoid arthritis, and autoimmune thyroiditis being the most common.
Q4. What role does inflammation play in post-COVID musculoskeletal disorders? Inflammation plays a crucial role in post-COVID musculoskeletal disorders. The initial cytokine storm during infection can lead to tissue damage, while persistent low-grade inflammation contributes to ongoing symptoms. This chronic inflammation can cause continued muscle and joint pain, fatigue, and other musculoskeletal issues.
Q5. What are some effective treatment options for post-COVID musculoskeletal symptoms? Effective treatment options include physiotherapy with graded exercise programs, anti-inflammatory medications (such as metformin or low-dose naltrexone), nutritional support to address deficiencies, and pain education with pacing strategies. A personalized rehabilitation plan that combines these approaches and monitors progress regularly is often most effective.