Shoulder arthritis affects up to 32.8% of adults over the age of sixty, making it one of the most common causes of shoulder pain and disability in older adults. When your shoulder joint’s smooth cartilage wears down, the resulting condition can severely limit your comfort and function. Most often occurring in people over age 50, shoulder arthritis can also develop in younger individuals following an injury or trauma, such as a shoulder fracture or dislocation.
Pain is the most common symptom you’ll experience with shoulder arthritis, often accompanied by stiffness, weakness, and a noticeable grinding sensation during shoulder movement. However, you don’t need to simply accept these limitations as inevitable. From non-surgical approaches like gentle stretching and anti-inflammatory medications to surgical options for severe cases, effective treatments are available. Throughout this guide, we’ll explore everything you need to know about shoulder arthritis, including its various types, how it differs from other shoulder conditions, and the best strategies for managing your symptoms and maintaining your quality of life.
Understanding Shoulder Arthritis
The degradation of cartilage within your shoulder joint defines shoulder arthritis. Your shoulder contains two primary joints, but shoulder arthritis typically refers to the larger ball-and-socket glenohumeral joint that connects your upper arm bone (humerus) to your shoulder blade (scapula). This protective cartilage covers both the ball (humeral head) and socket (glenoid), allowing smooth movement.
What is shoulder arthritis?
Shoulder arthritis occurs when the smooth cartilage lining your joint surfaces begins to break down, eventually leading to bone-on-bone contact. This cartilage breakdown creates a rough, uneven surface that causes pain, stiffness, and reduced function. As the condition progresses, bone spurs may form, further limiting motion. Patients often report that shoulder arthritis impacts their quality of life comparably to serious conditions like congestive heart failure or diabetes.
Types: Osteoarthritis, Rheumatoid, Post-traumatic
Several distinct types of shoulder arthritis exist, each with different origins:
- Osteoarthritis – The most common form, primarily affecting people over 50, this “wear and tear” arthritis gradually degrades cartilage through normal ageing processes. It affects up to 32.8% of patients over sixty and appears more common in women than men.
- Rheumatoid Arthritis – An autoimmune condition where your body attacks the synovial lining of joints, causing inflammation that damages cartilage. Unlike osteoarthritis, rheumatoid arthritis often affects both shoulders simultaneously.
- Post-Traumatic Arthritis – Develops after shoulder injuries like fractures or dislocations, which damage the cartilage surface.
Additional types include rotator cuff tear arthropathy (occurring after large rotator cuff tears) and avascular necrosis (when blood supply to the humeral head is disrupted).
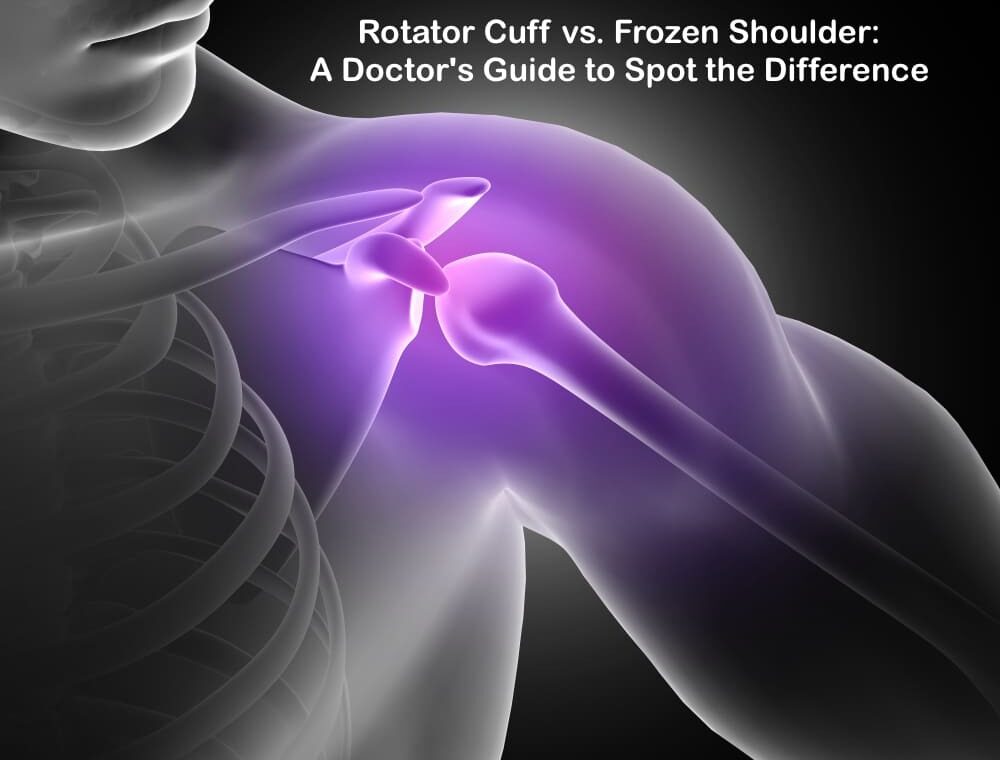
Shoulder arthritis vs frozen shoulder
Despite being commonly confused, shoulder arthritis and frozen shoulder (adhesive capsulitis) are entirely different conditions. The primary distinction lies in their underlying mechanisms:
Frozen shoulder specifically involves joint stiffness and chronic pain due to thickening and tightening of the joint capsule. In contrast, shoulder arthritis stems from cartilage deterioration. Furthermore, while arthritis causes pain but still allows some joint movement, frozen shoulder severely restricts mobility regardless of pain levels.
Understanding these differences is crucial since their treatments differ significantly, despite some overlapping symptoms.
Is your shoulder stiffness more than just ageing? Don't guess about your joint health. Get a precise diagnosis from an experienced Orthopedic Doctor in Mohali. Book Your Consultation Today or call us at +91 87250 11661.
Recognising the Signs and Symptoms
Recognising symptoms early helps manage shoulder arthritis effectively. Symptoms vary between individuals, with severity not always matching the degree of cartilage damage.
Early signs of shoulder arthritis
Initially, you might notice a dull ache in your shoulder that worsens after activities like lifting or reaching. Pain typically begins intermittently, appearing only during certain movements before becoming more constant as the condition progresses. Another early indicator is mild stiffness, particularly after periods of inactivity such as sleeping. Some individuals report occasional clicking sounds when moving their arms, even without pain.
Common symptoms: pain, stiffness, grinding
Pain remains the most common symptom of shoulder arthritis. As your condition advances, discomfort may occur at rest or during the night, making sleep difficult. The pain typically feels deep within the joint and can radiate down your arm toward your elbow or wrist.
Stiffness and reduced range of motion gradually increase, making everyday tasks like bathing or dressing challenging. Many patients experience crepitus—grinding, clicking, or popping sensations—when moving their shoulders. This occurs because cartilage loss creates uneven joint surfaces where bones rub together.
Shoulder arthritis vs rotator cuff tear
Although these conditions can coexist, they affect different structures. Shoulder arthritis primarily involves cartilage deterioration, whereas rotator cuff tears damage the tendons that position and power your joint. With rotator cuff tears, you’ll typically experience more pronounced weakness, especially during overhead activities. Moreover, rotator cuff tear arthropathy represents an advanced condition combining both problems, causing severe weakness, pain, and grinding.
Shoulder arthritis vs bursitis and tendinitis
Distinguishing between these conditions requires careful assessment. Bursitis involves inflammation of fluid-filled sacs (bursae) that cushion your joints. Comparatively, tendinitis affects the tendons connecting muscles to bones. Both can cause pain similar to arthritis, but differ in several ways:
- Location: Bursitis pain typically occurs at the top and outside of your shoulder, whereas arthritis pain originates within the joint itself.
- Duration: Bursitis generally resolves within weeks with proper care, while arthritis progressively worsens over time.
- Onset: Tendinitis often develops suddenly after repetitive activities, unlike the gradual onset of arthritis.
Pain and grinding in your shoulder shouldn't be ignored. Early intervention is key to preserving your mobility. Schedule an appointment with a Best Ortho Doctor in Mohali to discuss your symptoms and create a personalised management plan. Contact Our Ortho Clinic in Mohali Now.
Diagnosis and Imaging Techniques
Accurate diagnosis forms the cornerstone of effective shoulder arthritis treatment. Your doctor will employ a series of progressive diagnostic steps to pinpoint the exact nature and extent of your condition.
Physical examination and history
The diagnostic journey typically begins with a detailed conversation about your symptoms and medical history. Subsequently, your physician will conduct a thorough physical examination, checking for muscle weakness, tenderness to touch, and limited range of motion. They’ll assess both passive (assisted) and active (self-directed) shoulder movements. Notably, the doctor will listen for crepitus—a grinding sensation inside the joint during movement—which often indicates cartilage damage. The examination may include specific manoeuvres to evaluate your shoulder from multiple angles, including having you place your hands behind your head and back to assess rotation.
X-ray findings in shoulder arthritis
X-rays remain the first-line imaging technique for diagnosing shoulder arthritis. Key findings visible on X-rays include:
- Joint space narrowing (indicating cartilage loss)
- Bone spurs (osteophytes) along joint margins
- Subchondral sclerosis (increased bone density)
- Bone cysts beneath the joint surface
The axillary view provides the best angle to evaluate joint space narrowing, accordingly helping rule out dislocations. Your doctor may use the Kellgren-Lawrence score or Samilson and Prieto classification to grade the severity of your condition.
Shoulder arthritis MRI findings
Although not always necessary, MRI offers an exceptionally detailed evaluation of both soft tissues and bone. Typical MRI findings include cartilage thinning, bone marrow oedema, synovial thickening, and joint effusion. Furthermore, MRI excels at detecting rotator cuff tears that often accompany shoulder arthritis. This comprehensive assessment proves invaluable for surgical planning and detecting underlying causes of your condition.
When to consider lab tests
Laboratory tests become essential primarily when inflammatory arthritis is suspected. In certain cases, your doctor may analyse blood, urine, or joint fluid samples. Joint fluid analysis involves numbing the area before inserting a needle to withdraw fluid. These tests help differentiate between various forms of arthritis, particularly identifying inflammatory conditions like rheumatoid arthritis or ruling out infection.
Ready for a clear path to relief? Our clinic is equipped with advanced imaging technology to accurately diagnose your shoulder pain. Let the Best Orthopedician in Mohali guide your treatment. Visit our Google My Business Page to see reviews and call us to get started.
Treatment Options and Management
Treatment approaches for shoulder arthritis range from conservative options to surgical interventions, depending on pain severity and functional limitations. A comprehensive management plan typically begins with the least invasive methods first.
Non-surgical management of shoulder arthritis
First and foremost, optimising your overall health can improve the quality of life with shoulder arthritis. Regular aerobic exercise, maintaining a healthy weight, and avoiding activities that worsen pain form the foundation of management. Gentle stretching exercises help maintain range of motion, thus preventing further stiffness. Applying ice reduces inflammation, while heat can loosen stiff joints. Physical therapy often plays a crucial role in preserving mobility without aggravating symptoms.
Shoulder arthritis injection – Steroid, PRP, Hyaluronic Acid
Corticosteroid injections can provide significant short-term relief by reducing inflammation. Nevertheless, most doctors limit these to three injections yearly to prevent cartilage damage. Hyaluronic acid injections mimic your joint’s natural lubricant, potentially offering pain relief lasting up to six months. Meanwhile, platelet-rich plasma (PRP) therapy uses your own blood components to potentially promote healing, though research shows mixed results.
Pain relief for shoulder arthritis
Over-the-counter medications like acetaminophen offer basic pain control with fewer side effects than other options. Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen reduce both pain and inflammation. Certainly, medication should complement rather than replace other treatment approaches. For nighttime pain, icing the shoulder before bed may improve sleep quality.
Shoulder arthritis supplements
Certain supplements show promise for arthritis management. Glucosamine and chondroitin have produced mixed research results. In fact, turmeric/curcumin demonstrates anti-inflammatory properties, with one study showing effectiveness comparable to ibuprofen. Additionally, fish oil contains omega-3 fatty acids that help block inflammatory compounds. Remember to discuss any supplements with your physician, as they may interact with medications.
Shoulder arthritis surgical options
When conservative measures fail, surgical options include arthroscopic debridement for early arthritis, which removes loose tissue fragments. Total shoulder replacement replaces both the ball and socket with artificial components, effectively eliminating arthritis pain. For patients with combined rotator cuff tears and arthritis, reverse total shoulder replacement may provide better outcomes.
Shoulder arthritis recovery time and prognosis
Recovery from shoulder replacement typically requires wearing a sling for 4-6 weeks. Most people resume light activities after 2-3 weeks. Physical therapy continues for approximately 12 weeks, focusing initially on flexibility, then progressing to strength. Fortunately, 95% of patients experience pain-free function one year after surgery. Many prosthetic shoulders last at least 15 years, often for the remainder of a patient’s life.
From non-surgical therapies to advanced joint replacement, explore all your options for Orthopedic Treatment in Mohali. Don't let pain dictate your life. Take the first step towards a pain-free shoulder. Click here to consult with the Best Orthopedic Doctor in Mohali.
Conclusion
Living with shoulder arthritis certainly presents challenges, but knowledge empowers you to take control of your condition. Throughout this guide, we’ve explored how shoulder arthritis develops when protective cartilage deteriorates, leading to pain, stiffness, and reduced mobility. Remember that several types exist—osteoarthritis, rheumatoid arthritis, and post-traumatic arthritis—each requiring specific approaches.
Early recognition of symptoms allows for prompt intervention. Pain, stiffness, and grinding sensations warrant medical attention, especially when they persist or worsen. Your doctor will likely use physical examinations, X-rays, and sometimes MRIs to accurately diagnose your condition.
Treatment options span a wide spectrum based on your specific needs. Conservative approaches like gentle stretching, heat and ice application, and physical therapy often provide significant relief. Medications and injections serve as effective tools for managing pain and inflammation. When these methods prove insufficient, surgical interventions such as debridement or joint replacement can dramatically improve your quality of life.
Many patients worry about their future with shoulder arthritis. However, modern treatment approaches yield excellent outcomes. After surgery, most people return to normal activities within weeks, and the long-term prognosis remains positive with proper care. Whether you’re newly diagnosed or have battled shoulder pain for years, effective management strategies exist.
Shoulder arthritis doesn’t need to define your life. Armed with proper information and working alongside healthcare providers, you can minimise pain, maintain mobility, and continue enjoying meaningful activities despite this condition. Your journey with shoulder arthritis may require adjustments, but it need not end the activities that bring you joy.
Key Takeaways
Understanding shoulder arthritis empowers you to recognise symptoms early and pursue effective treatment options that can significantly improve your quality of life.
• Early recognition matters: Watch for persistent shoulder pain, stiffness after inactivity, and grinding sensations during movement—these often signal developing arthritis.
• Multiple treatment paths exist: From gentle stretching and anti-inflammatory medications to injections and surgery, effective options are available for every severity level.
• Conservative care works first: Physical therapy, ice/heat application, and maintaining a healthy weight can provide significant relief without invasive procedures.
• Surgery offers excellent outcomes: 95% of patients experience pain-free function one year after shoulder replacement, with most prosthetics lasting 15+ years.
• Don’t accept limitations: With proper diagnosis and treatment, shoulder arthritis doesn’t have to prevent you from enjoying meaningful activities and maintaining an active lifestyle.
The key is working with healthcare providers to develop a personalised management plan that matches your specific type of arthritis and lifestyle needs. Whether through conservative care or surgical intervention, effective relief is achievable.
FAQs
Q1. At what age does shoulder arthritis typically develop?
A1. Shoulder arthritis most commonly affects individuals over 50 years old. However, it can also occur in younger people, particularly following shoulder injuries or trauma. The condition tends to progress gradually over time.
Q2. What are the early warning signs of shoulder arthritis?
A2. Early signs include a dull ache in the shoulder that worsens with activity, mild stiffness (especially after periods of inactivity), and occasional clicking sounds during arm movement. As the condition progresses, pain may become more constant and affect sleep.
Q3. How is shoulder arthritis diagnosed?
A3. Diagnosis typically involves a physical examination, review of medical history, and imaging tests. X-rays are the primary diagnostic tool, showing joint space narrowing and bone spurs. In some cases, MRI scans may be used for a more detailed evaluation of soft tissues and bone.
Q4. What non-surgical treatments are available for shoulder arthritis?
A4. Non-surgical options include gentle stretching exercises, physical therapy, ice/heat application, and pain relief medications. Corticosteroid injections can provide short-term relief. Some patients find benefit from supplements like glucosamine or turmeric, though results vary.
Q5. What is the recovery process like after shoulder replacement surgery?
A5. After shoulder replacement, patients typically wear a sling for 4-6 weeks. Light activities can often resume after 2-3 weeks. Physical therapy continues for about 12 weeks, focusing first on flexibility, then strength. Most patients experience pain-free function within a year, with prosthetic shoulders often lasting 15 years or more.
Your journey to a pain-free life starts with a single step. Trust your care to a specialist dedicated to restoring your mobility. For expert Orthopedic Treatment in Mohali, reach out to us.
📞 Call Now: +91 87250 11661 | ⭐ See Patient Reviews: Our Google My Business Profile